Radiation accidents occur under several different potential circumstances which may involve different numbers of people. Good examples are the Goiania Accident involving a few hundred people (Oliveira et al. 1991) and the Chernobyl (NEA 2002) and Fukushima (NERH 2011) nuclear accidents involving hundreds of thousands of people. Radiation incidents can also be caused deliberately, as a result of terrorist actions. The emergency consequences depend not only on the number of injuries and types of exposure, but also on the emergency management. In all cases preparedness for this kind of event is crucial. A large number of injured people will require many laboratories capable of providing assistance to the national emergency preparedness organization in the country where the accident occurred.
The RENEB project (Kulka et al. 2016) was launched in 2012 with the aim to establish a sustainable network in biological and physical-retrospective dosimetry that involves a large number of experienced laboratories throughout the European Union (EU). The network enables the activation of many laboratories immediately after a radiological emergency. Samples collected during an emergency can be sent to laboratories which are ready to give their assistance in provision of individual dose estimates. This possibility decreases the time for specification of doses, provided that all laboratories are prepared and trained. Moreover, reporting of dosimetric results must be organized in a consistent manner.
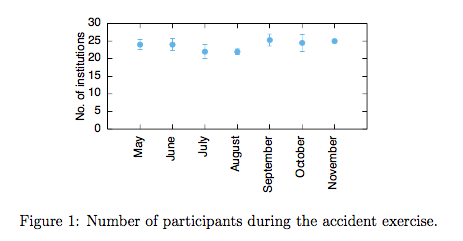
 The RENEB accident exercise was performed as a last exercise within WP1: Operational Basis. It was launched on 18th of May 2015 and ended on 6th of December 2015. There were 28 institutes participating in the exercise: 21 RENEB members, 4 candidates and 4 non-RENEB partners. The aim of the accident exercise was to test the procedure of activating the RENEB network in case of a radiological event. 27 exercises were performed during 27 weeks, starting from May and ending in December 2015. The number of laboratories taking part in each exercise varied as shown in Fig. 1, but was never below 64% of the total number.
The RENEB accident exercise was performed as a last exercise within WP1: Operational Basis. It was launched on 18th of May 2015 and ended on 6th of December 2015. There were 28 institutes participating in the exercise: 21 RENEB members, 4 candidates and 4 non-RENEB partners. The aim of the accident exercise was to test the procedure of activating the RENEB network in case of a radiological event. 27 exercises were performed during 27 weeks, starting from May and ending in December 2015. The number of laboratories taking part in each exercise varied as shown in Fig. 1, but was never below 64% of the total number.
The RENEB project (Kulka et al. 2016) was launched in 2012 with the aim to establish a sustainable network in biological and physical-retrospective dosimetry that involves a large number of experienced laboratories throughout the European Union (EU). The network enables the activation of many laboratories immediately after a radiological emergency. Samples collected during an emergency can be sent to laboratories which are ready to give their assistance in provision of individual dose estimates. This possibility decreases the time for specification of doses, provided that all laboratories are prepared and trained. Moreover, reporting of dosimetric results must be organized in a consistent manner.
 The RENEB accident exercise was performed as a last exercise within WP1: Operational Basis. It was launched on 18th of May 2015 and ended on 6th of December 2015. There were 28 institutes participating in the exercise: 21 RENEB members, 4 candidates and 4 non-RENEB partners. The aim of the accident exercise was to test the procedure of activating the RENEB network in case of a radiological event. 27 exercises were performed during 27 weeks, starting from May and ending in December 2015. The number of laboratories taking part in each exercise varied as shown in Fig. 1, but was never below 64% of the total number.
The RENEB accident exercise was performed as a last exercise within WP1: Operational Basis. It was launched on 18th of May 2015 and ended on 6th of December 2015. There were 28 institutes participating in the exercise: 21 RENEB members, 4 candidates and 4 non-RENEB partners. The aim of the accident exercise was to test the procedure of activating the RENEB network in case of a radiological event. 27 exercises were performed during 27 weeks, starting from May and ending in December 2015. The number of laboratories taking part in each exercise varied as shown in Fig. 1, but was never below 64% of the total number.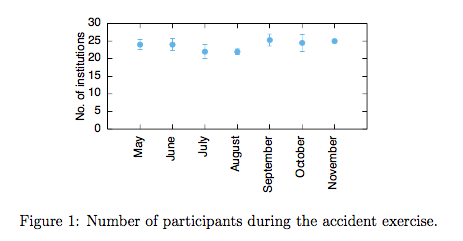
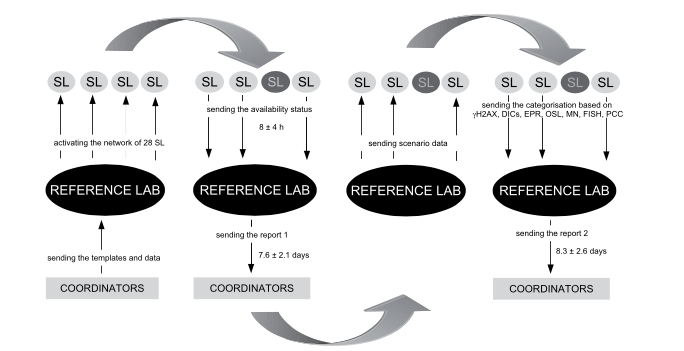
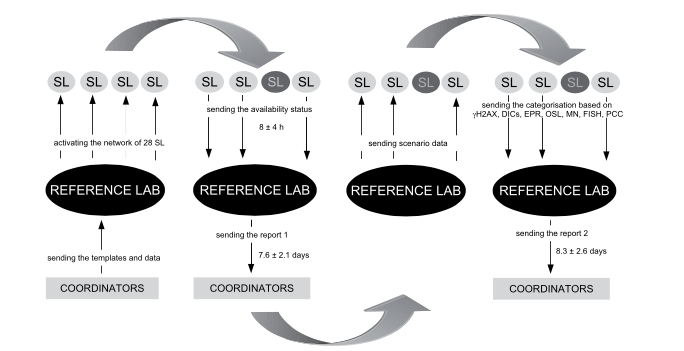
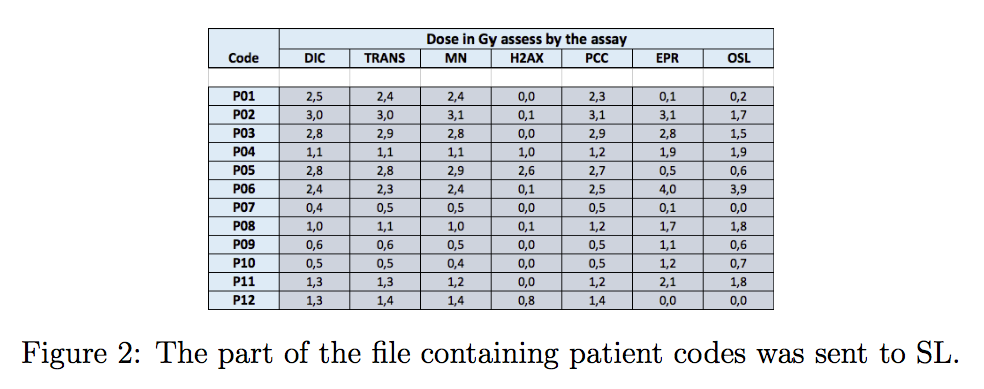
The exercise was virtual and organised for the first time in such scale. Activating the network was based on e-mail exchanges only, because physical analyses of blood samples were done during two previous inter-comparisons. Moreover, the aim was to test and train the procedures associated with activating the network in case of an emergency. Two types of laboratories were introduced: RL (Reference Laboratory) and SL (Service laboratory). Each week a RL activated the network by sending e-mails to all SL and asking them for help to analyse blood samples of exposed people. If a SL was available, the SL team leader sent a response including the capacity of his/her laboratory. Next, the RL sent virtual samples to the available SL. Virtual samples were in fact Excel files with dosimetric information from all RENEB assays per an exposed person. Each file included 54 patient codes with 10 doses estimated by the following assays: dicentrics - DICs (man, auto), chromosome painting - FISH, micronuclei - MN (man, auto), gamma-H2AX (man, auto), premature chromosome condensation - PCC, electron paramagnetic resonance - EPR and optically stimulated luminescence - OSL. An example of a dose data set for 12 patients is shown in Fig. 2.
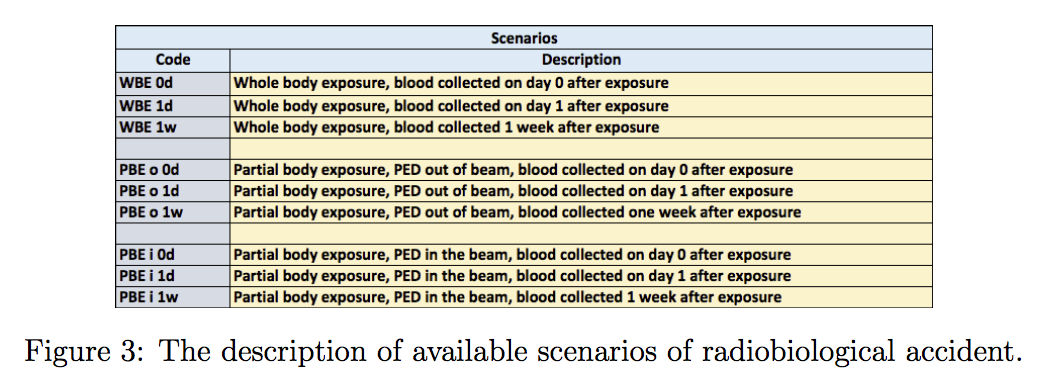
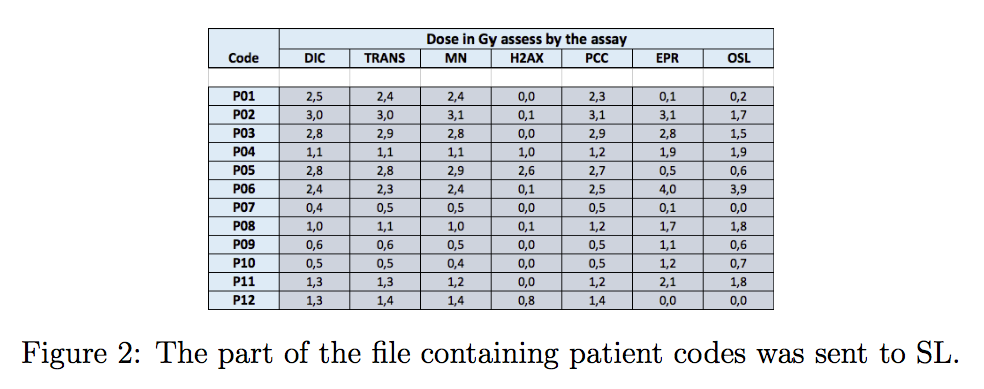 Generally, the task of a SL was to return the information regarding the capacity of the SL (in terms of blood sample number) and to classify each patient according to given rules. The first rule was to triage the person as green (for doses less than 1 Gy), orange (between 1 and 2 Gy) and red (more than 2 Gy). Additionally, the SL was asked to estimate the exposure scenario. For this purpose 9 scenarios were introduced as shown in Fig. 3. The final decision about a scenario was on combining the information from all assays, even if the assay itself was not performed by the SL.
Generally, the task of a SL was to return the information regarding the capacity of the SL (in terms of blood sample number) and to classify each patient according to given rules. The first rule was to triage the person as green (for doses less than 1 Gy), orange (between 1 and 2 Gy) and red (more than 2 Gy). Additionally, the SL was asked to estimate the exposure scenario. For this purpose 9 scenarios were introduced as shown in Fig. 3. The final decision about a scenario was on combining the information from all assays, even if the assay itself was not performed by the SL.
 In total, there were 27 weekly exercises which means that only one laboratory declined to participate as a Reference Laboratory. RL was responsible for activating the network, but the RL leader also had to prepare two reports gathering all SL data and to send it to the exercise coordinator. The first report included information about the SL capacity. The second report was a combination of all SL triage estimations. The mean time of receiving report 1 was around 7.5 days while the time of sending report 2 was 8.3 days.
In total, there were 27 weekly exercises which means that only one laboratory declined to participate as a Reference Laboratory. RL was responsible for activating the network, but the RL leader also had to prepare two reports gathering all SL data and to send it to the exercise coordinator. The first report included information about the SL capacity. The second report was a combination of all SL triage estimations. The mean time of receiving report 1 was around 7.5 days while the time of sending report 2 was 8.3 days.
The results were published in International Journal of Radiation Biology in January 2017.
 Generally, the task of a SL was to return the information regarding the capacity of the SL (in terms of blood sample number) and to classify each patient according to given rules. The first rule was to triage the person as green (for doses less than 1 Gy), orange (between 1 and 2 Gy) and red (more than 2 Gy). Additionally, the SL was asked to estimate the exposure scenario. For this purpose 9 scenarios were introduced as shown in Fig. 3. The final decision about a scenario was on combining the information from all assays, even if the assay itself was not performed by the SL.
Generally, the task of a SL was to return the information regarding the capacity of the SL (in terms of blood sample number) and to classify each patient according to given rules. The first rule was to triage the person as green (for doses less than 1 Gy), orange (between 1 and 2 Gy) and red (more than 2 Gy). Additionally, the SL was asked to estimate the exposure scenario. For this purpose 9 scenarios were introduced as shown in Fig. 3. The final decision about a scenario was on combining the information from all assays, even if the assay itself was not performed by the SL.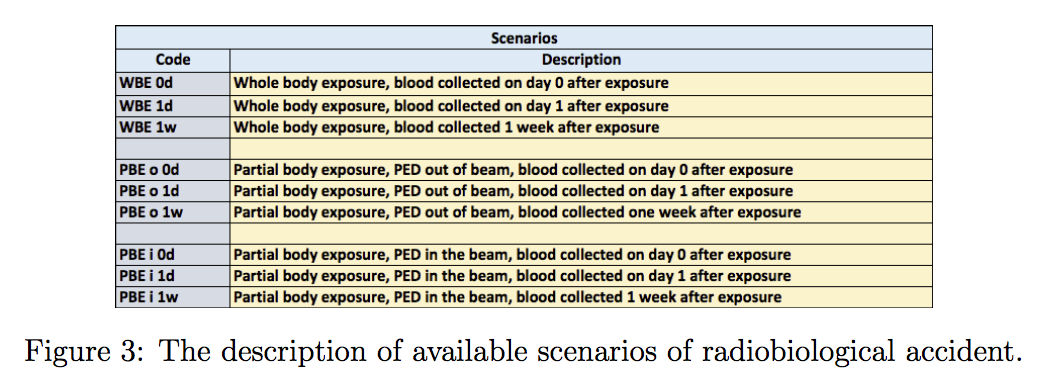 In total, there were 27 weekly exercises which means that only one laboratory declined to participate as a Reference Laboratory. RL was responsible for activating the network, but the RL leader also had to prepare two reports gathering all SL data and to send it to the exercise coordinator. The first report included information about the SL capacity. The second report was a combination of all SL triage estimations. The mean time of receiving report 1 was around 7.5 days while the time of sending report 2 was 8.3 days.
In total, there were 27 weekly exercises which means that only one laboratory declined to participate as a Reference Laboratory. RL was responsible for activating the network, but the RL leader also had to prepare two reports gathering all SL data and to send it to the exercise coordinator. The first report included information about the SL capacity. The second report was a combination of all SL triage estimations. The mean time of receiving report 1 was around 7.5 days while the time of sending report 2 was 8.3 days.The results were published in International Journal of Radiation Biology in January 2017.
OUR TEAM
- Ulrike Kulka, RENEB leader
- Andrzej Wójcik, WP coordinator
- Beata Brzozowska, task coordinator